Types Of Vaccines
How vaccines work
Last week we mentioned the importance of vaccination and the reasons that we can trust the studies supporting their use. We also mentioned a couple of countries that have successfully eradicated infectious diseases with vaccination programmes.
There are hundreds of countries that no longer deal with horrific diseases thanks to vaccination, but some people are hesitant or resistant still. To help ease the anxiety of anyone confused about vaccines – for COVID or generally – we are going to focus on how they work this week.
Most people with a general understanding of vaccination science know vaccines to contain a small amount of the disease they are used to treat. While that is true of one type of vaccine, there are other, more modern, varieties that work differently.
Messenger RNA (mRNA) vaccines
One of the main types of vaccines used to prevent COVID-19 is the messenger RNA (mRNA). Instead of injecting people with part of a pathogen, mRNAs contain a set of instructions for the immune system to simulate their response. These instructions tell our cells to produce a part of a virus, like the spike proteins (in the case of Covid-19). Once spike proteins are produced, our body’s immune system is then stimulated to produce antibodies to fight against it. Once the antigens exist, the immune system hopefully holds on to their learnings for the next time that disease appears.
This is an incredibly safe type of vaccine because it contains no real virus. mRNAs cannot alter our DNA, as some anti-vaccination propaganda might claim, because it does not reach the nucleus of our cells – which is where our DNA is stored.
mRNA vaccines contain no live virus. They elicit a strong immune response and have no chance of replicating the wild disease. An example is pfizer COVID-19 vaccine.
Virus vector vaccines
Another type of vaccine used to fight COVID-19 is the virus – or viral – vector. Like mRNAs, these carry instructions to the cells to tell them to produce the relevant spike proteins and antigens for the disease being vaccinated against.
These antigens trigger an effective immune response that the body remembers after just one dose. The virus vector is a very safe type of vaccine because and our body is used to targeting the modified virus.
Despite being safe and effective, they are expensive to produce and may be less effective on anyone that has already had exposure to the wild virus.
Viral vector vaccines use a harmless alternative virus. They elicit a strong immune response and have no chance of replicating the wild disease. An example is COVID Astra Zeneca.
Inactivated vaccines
Inactivated vaccines are a low-risk alternative to live-attenuated types, where the virus or bacteria is killed before use. This is preferable for diseases where the risk of live infection is high.
The disadvantage of inactivated vaccines is that the immune response they trigger is weaker. Usually, this can be worked around by giving multiple doses of the vaccine (for example, the HPV jab which requires 3 doses for over 15s).
Inactivated vaccines use a dormant virus. They elicit a weaker immune response but have no chance of replicating the wild disease, making them much safer. Examples are flu, hep A and polio shot.
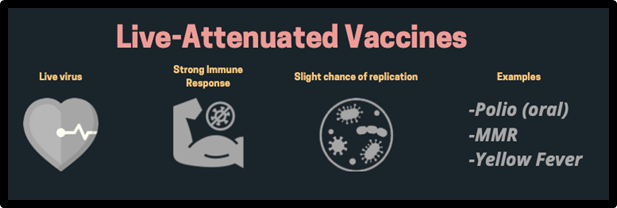
Live-attenuated vaccines
The best-known and first type to be made is the live vaccine. It contains a tiny amount of a weakened live virus or bacteria. Because it is weak, our immune systems can easily fight it off (but we may still get some side effects), but our body still recognises and responds to it.
This weak virus trains our immune system to fight off the more dangerous version of itself. When the immune system destroys a virus for the first time, it creates antigens that it can quickly recognise and destroy next time – when the virus is stronger.
Because live-attenuated vaccines rely on a strong immune system, they are not suitable for immunocompromised people. They are also not normally used for people who are pregnant. To protect those that cannot be vaccinated, the rest of the population must reach the threshold needed for herd immunity.
The main disadvantage of live-attenuated vaccines is the extremely unlikely possibility that the full virus can be replicated in the body.
Live-attenuated vaccines use a weakened live virus. They elicit a strong immune response but have a small chance of replicating the wild disease. Examples are oral polio, MMR and yellow fever.
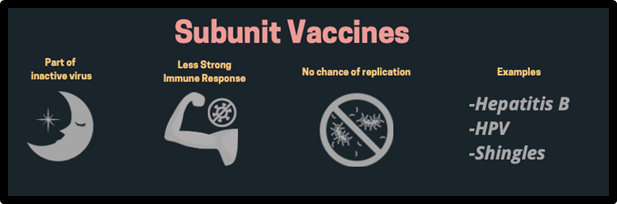
Subunit vaccine
Subunit vaccines use part of an inactive virus or bacteria cell to trigger an immune system response. Because it uses only a small part, the response is strong and targeted. So, when the entire cell enters the body in the future, the immune system will destroy that part, killing the cell.
These types of vaccines are harmless because they contain the antigens needed but not the symptom-producing parts of the cell. They are effective but require boosters for an ongoing effect.
Subunit vaccines use a part of a dormant virus. They elicit a weaker immune response but have no chance of replicating the wild disease, so are much safer. Examples are hep B, HPV and Shingles.
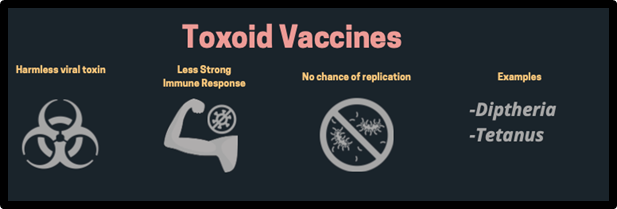
Toxoid vaccines
Toxoid vaccines use a toxin made by the cells of a disease. They teach the immune system to destroy the parts of the cells that produce symptoms but leave the rest of the cell unharmed.
This is useful for non-contagious diseases with harmful symptoms, where the symptoms are the part of the virus that is deadly. Toxoid vaccines are incredibly safe because they contain no live bacteria so cannot cause the disease they fight. They also rarely produce adverse reactions.
Viral vector vaccines use a harmless viral toxin. They elicit a weaker immune response but have no chance of replicating the wild disease. Examples are diphtheria and tetanus.
Types of vaccines and how they work
We hope this has helped you to understand the science behind some of the main types of vaccination. While some types are relatively new, the research behind them has been going on for decades. The COVID-19 vaccine – like all others – is safe and effective.
If you would like to arrange vaccination for COVID or any other disease, or if you have concerns about any vaccine, reach out to your doctor who can answer your questions in more detail.
For more information, the Australian Health Department has produce some very well researched and balanced resources especially for Covid-19 vaccines. They can be found here: https://www.health.gov.au/initiatives-and-programs/covid-19-vaccines
Felicity Thompson
and